Check back weekly for the latest survey results and updates.
For last week's data, see Week 2 Results.
Who replied to the survey in Week 3?
The number of respondents to the survey continues to grow. This week, 713 primary care physicians, nurse practitioners, and PAs took the survey, representing a range of specialties: family medicine (59%), geriatrics (13%), internal medicine (12%), primary care-based pharmacists and behavioral health (11%), and pediatrics (5%). Responses were received from all 50 states plus American Samoa. A fifth of respondents work in small practices (≤ 3 clinicians), a third work in practices owned by an academic medical center, and about a fifth own their practices. Twenty-three percent of week 3 respondents practice in a rural setting.
Responses to week 3 of the survey were collected March 27-30, 2020.
Results at a glance
Nearly 8 in 10 clinicians report their practice is under “severe” or “close to severe” strain due to COVID-19.
Forty-five percent of respondents classify the level of strain on their practice as “severe” (level 5 on a 1-to-5 scale) and another 35% classify it as “close to severe” (level 4) strain. These combined numbers largely held steady from week 2.
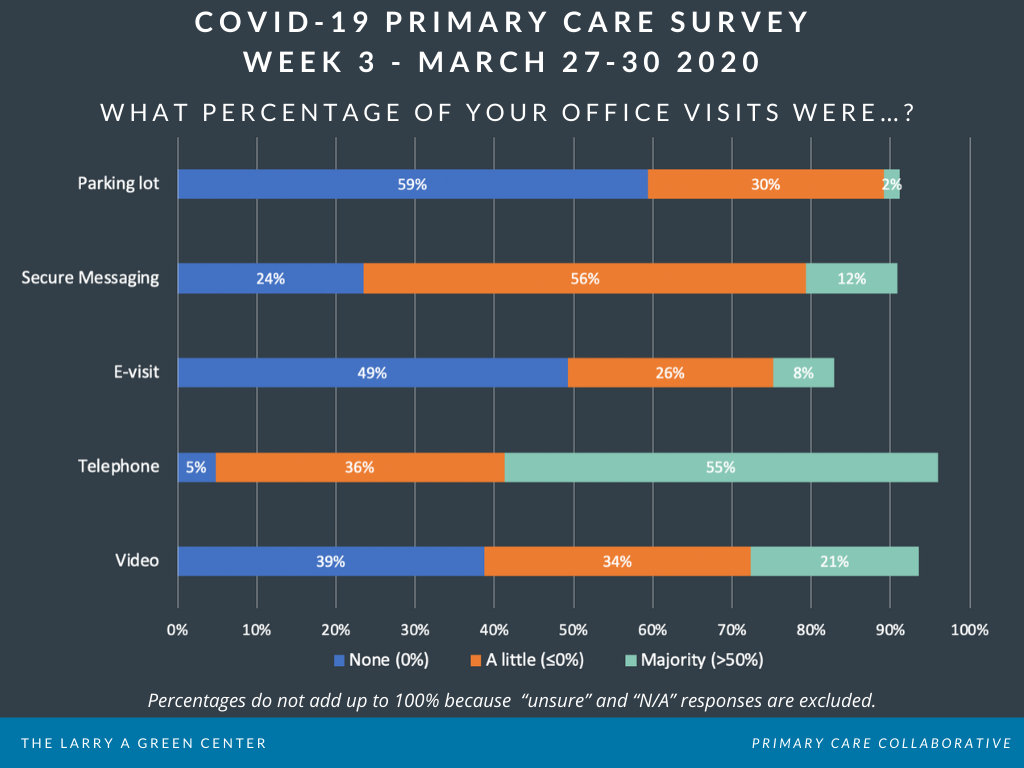
Video and other telehealth capacity is increasing, though it’s still far from standard.
In week 3, 39% of respondents report that their practice has NO video visits (down from 60% the week before). About half (49%) report that NO e-visits are occurring at their practice (down from 70% the week before).
Over half of primary care practices are conducting the majority of their visits by telephone.
Fifty-five percent of clinicians say that their practice is conducting ≥50% of their patient visits by telephone.
Nearly a third of respondents work at practices that offer some visits in the parking lot.
Thirty-two percent say that at least some visits are being handled in the parking lot outside the office, though only 2% work at practices that are conducting the majority of their visits there.
Only a third of primary care clinicians feel sure that their practice has enough cash on hand to function for four weeks.
Thirty-four percent of respondents answered “yes”, and another 15% said “maybe”. Half answered either “no” (13%) or “unsure” (37%).
Nearly a quarter of respondents report that their practice may need to temporarily close.
Reasons for possible temporary closure included: “clinician or staff illness” (20% maybe; 2% yes); “lack of PPE/supplies" (21% maybe; 3% yes); and “lack of revenue” (16% maybe; 2% yes).
Voices from the Primary Care Front Lines
252 clinicians provided open text comments in the week 3 survey.
Many described the immediate and long-term financial strain on practices
- “There is an increasing likelihood that my practice will financially fail over the next 4 weeks. I am in a solo practice but part of a larger group. We are being told to lay off employees. I am overrun with prescription refills and prior [authorizations] for medications and normal calls (all of which is uncompensated) ...I fear at a time when I will be most needed, my practice will no longer be around.” (Virginia)
- “When 50% of private practice PCPs go out of business, how will we EVER control health care costs? The answer we won't. Private practice PCPs are going to die without help.” (Michigan)
- “We furloughed a large percentage of our organization due to lost revenue.” (Connecticut)
Comments highlighted telehealth challenges—from payment to patient access
- “We are setting up telehealth as quickly as possible with no idea how much or if we will get paid.” (Missouri)
- “Patients most vulnerable don’t have telemedicine access.” (Alaska)
- “Encountering a huge issue with the Payers who are currently refusing to pay for Telehealth visits by our [Advanced Practice Providers (APPs)] if the visit is conducted from the APP's home instead of the office.” (Virginia)
Respondents shared alarming descriptions of PPE and testing shortages
- “We are only handling emergencies over the phone- we cannot get sufficient PPE so we can't go to the office. The state is taking what little we have for the hospital.” (New Jersey)
- “I have been using the same mask for a week. My nursing staff are sharing 1 mask depending on how close their contact is with patients. This is unacceptable, but we either close or continue to expose ourselves to illness. Few hospices willing to accept patients w/COVID-some due to lack of PPE.” (Texas)
- “It is criminal to have healthcare workers risking their lives due to reluctance of the federal government to take charge of mandating production of PPE and patient support items (e.g., ventilators).” (New Hampshire)
Still, many comments spoke to bright spots: staff resilience and “an amazing rate of change” in how practices handle care
- “We have had awesome system response - set up triage line with 1500 patient calls per day, switched to virtual visits within one week, etc.” (Colorado)
- “Hospital operations team working collaboratively with primary care leaders, ED; designed parking lot testing centers, clinician pools for callbacks, patient education, expanded hospital care teams.” (Pennsylvania)
- “I've been completely humbled by the resilience and adaptability of everyone in the organization.” (Virginia)
Learn more: Download the Week 3 Executive Summary.
| Attachment | Size |
|---|---|
| 121.5 KB |

Are you a physician, nurse practitioner, or PA working in primary care?
Help PCC and the Larry A. Green Center track how your practice is responding to the COVID-19 outbreak by completing the Green Center's occasional survey.
The regular surveys are no longer being conducted.
COVID-19 Updates
May 9, 2022 | Primary Care Collaborative
April 19, 2022 | Primary Care Collaborative
April 19, 2022 | Primary Care Collaborative
March 7, 2022 | STAT
February 27, 2022
- 1 of 39
- next ›

Recent News
April 22, 2024
March 19, 2024
February 28, 2024
February 22, 2024 | Conversations on Health Care
May webinar highlights: “The Commercial Market: Alternative Payment Models for Primary Care” Nate Murray explains w… https://t.co/KX9Wi2w6oY —
10 months 2 weeks ago
@CMSinnovates’ primary care strategy is rooted in a 2021 @theNASEM’s report which called #primarycare “foundational… https://t.co/glbPxvCysg —
10 months 2 weeks ago
@CMSinnovates has a new #primarycare strategy, envisioning “ACO-based primary care model tests that may focus on pr… https://t.co/aJGF1z411l —
10 months 2 weeks ago
- Page 1
- ››
Secondary menu
Copyright © 2024 Primary Care Collaborative