U.S. primary care is failing patients due to a clinician shortage and chronic underinvestment, leaving a growing share of Americans unable to establish a regular primary care relationship. A new report from the Primary Care Collaborative (PCC) and the Robert Graham Center says solving this crisis requires a new payment approach and more and more diverse healthcare professionals to enter the field.
According to the report, Health is Primary: Charting a Path to Equity and Sustainability, the United States has seen a consistent decrease in the number of primary care clinicians since 2014, caused by a decline in the number of clinicians entering primary care, burnout leading to retirement, and decreased direct patient care time. In 2019, there was a net loss of 10 clinicians per 100,000 people across the US. Spending on primary care fell from an average of 6.2% in 2013 to 4.6% in 2020.
“Hi-tech healthcare grabs the headlines, but hi-touch, personalized primary care with tech support keeps people healthier at a lower cost,” said Ann Greiner, president and CEO of PCC. “If we are serious about improving the health of everyone in every community, policymakers need to step up to strengthen primary care, making it attractive to clinicians and delivering what patients want – comprehensive team-based care.
Experts recommend a multifaceted approach to rebuilding primary care that outlines steps policymakers, providers, and employers can take, including:
- Offering more primary care training opportunities and incentives for clinicians to select primary care as a specialty,
- Collecting accurate and transparent workforce and primary care financing data,
- Establishing a hybrid primary care payment option alternative to fee-for-service for accountable care organizations (ACOs) in the Medicare Shared Savings Program (MSSP) and more broadly across public and private programs,
- Crafting solutions to mitigate the primary care barriers of high deductible health plans, and
- Supporting today’s primary care workforce by lowering administrative burdens and building diverse teams to address the range of patient primary care needs.
Having access to a regular source of primary care is associated with fewer emergency department visits and hospitalizations, lower odds of dying prematurely, and lower healthcare costs. Data from MSSP, Medicare’s largest ACO program serving 11 million beneficiaries, consistently indicates that primary care-focused ACOs provide higher-value services and produce the lion’s share of the $1.8 billion Medicare savings realized in 2022.
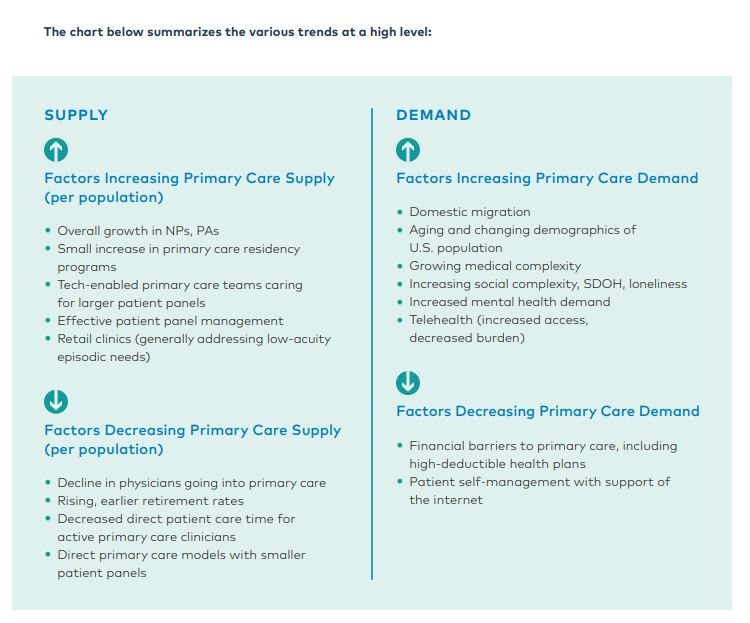
The report examines the supply and demand factors that contribute to primary care access issues including:
It also considers innovations such as direct primary care, telehealth, and retail clinics that aim to provide more equitable access but may pose unintended community-level financial burdens and access issues. Despite increased uptake of these care options, one-in-four U.S. residents currently do not have a relationship with a primary care clinician, and 40% of adults in the United States failed to have a primary care visit in 2019. These trends have been exacerbated by the COVID-19 pandemic, suggesting that the situation may be more dire than the report’s data reflect.
“The United States lacks the physicians and other clinicians needed to ensure that the front door of the nation’s health care system remains open,” said Alison N. Huffstetler, MD, medical director at the Robert Graham Center. “Recently, U.S. life expectancy declined by two years – worse for those without college degrees and from lower socioeconomic neighborhoods – and we will not reverse these declines unless we strengthen primary care.”
About the Primary Care Collaborative
Founded in 2006, the Primary Care Collaborative (PCC) is a not-for-profit multi-stakeholder membership organization dedicated to advancing an effective and efficient health system built on a strong foundation of primary care and the patient-centered medical home. Representing a broad group of public and private organizations, PCC’s mission is to unify and engage diverse stakeholders in promoting policies and sharing best practices that support growth of high-performing primary care and achieve the “Quadruple Aim:” better care, better health, lower costs, and greater joy for clinicians and staff in delivery of care. For more information about PCC, visit www.pcpcc.org.
About the Robert Graham Center
The Robert Graham Center aims to improve individual and population healthcare delivery through the generation or synthesis of evidence that brings a family medicine and primary care perspective to health policy deliberations from the local to national levels.
Recent News
April 30, 2024
April 22, 2024
Missed our May webinar, “The Commercial Market: Alternative Payment Models for Primary Care,” check out this clip!… https://t.co/mDZH3IINXK —
11 months 1 day ago
Did you catch @CMSinnovates' new #primarycare strategy? Thanks to concerted efforts from @NAACOSnews and other memb… https://t.co/mDnawqw8YW —
11 months 1 day ago
Not up to date on the #Medicaid Access and #Managedcare proposed rules important for #primarycare? No worries,… https://t.co/qB6sY3XCZ1 —
11 months 4 days ago
Secondary menu
Copyright © 2024 Primary Care Collaborative