Accountable Care Organizations (ACOs)
Accountable Care Organizations (ACOs)
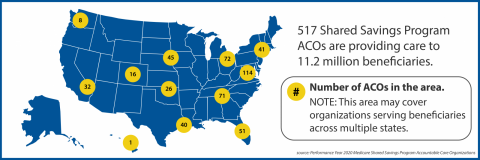
ACOs are defined by the Center for Medicare and Medicaid Services (CMS) as groups of doctors, hospitals, and other health care providers, who come together voluntarily to give coordinated high-quality care to their Medicare patients. The goal of coodinated care is to ensure that patients get the right care at the right time, while avoiding unnecessary duplication of services and preventing medical errors.
When an ACO succeeds both in delivering high-quality care and spending health care dollars more wisely, the ACO will share in the savings it achieves for the Medicare program.
The PCC believes that primary care is the foundation of a successful ACO that uses transparent performance measures to achieve the Quadruple Aim of improving population health, improving patients' experience of care, reducing the total cost of care, and improving the work life of health care providers. In an ACO, strong primary care physician leadership of the care team is necessary to improve care coodination, and enhance preventitive care delivery.
For more information about ACO's visit the American Academy of Family Physicians (AAFP) website
Resources
Payment Methods and Benefit Designs: How They Work and How They Work Together to Improve Health Care
Urban Institute & Catalyst for Payment Reform | May 2016
This resource discusses a project conducted that looks at how payment methods and benefit designs can work together to improve quality and increase value of care. This intersection should be considered when moving forward with reforms that aim to create more high-value care.

The Patient-Centered Medical Home's Impact on Cost and Quality: Annual Review of Evidence, 2014-2015
Patient-Centered Primary Care Collaborative | February 2016

Pediatric Medical Home Infographic-Responding to Change | November 2015

American Journal of Managed Care | October 2015

JAMA Internal Medicine | September 2015
This study looks at how accountable care organizations (ACOs) improve healthcare efficiency by decreasing the provision of low-value care that provides minimal clinical benefits. It concluded that these type of risk-contracts may discourage use of low-value services and lead to more high-value care.
- ‹ previous
- 3 of 18
- next ›
News
August 12, 2020 | Kaiser Health News
October 21, 2019 | Health Affairs Blog
October 8, 2019 | The Boston Globe
- ‹ previous
- 3 of 54
- next ›
Events & Media
April 11, 2019 | America's Physician Groups
October 10, 2018 | Remedy Partners
- ‹ previous
- 3 of 30
- next ›
Related Content
Pages
Pages
Pages
- « first
- ‹ previous
- 1
- 2
- 3
Secondary menu
Copyright © 2024 Primary Care Collaborative