Payment Reform
Various payment innovations have been testing ways to support primary care innovation and PCMH for many years. Depending on the region and the provider arrangement (e.g., a solo or small practice, an Independent Practice Association or Accountable Care Organization (ACO), or an employed provider as part of a health system), some practices that were once paid fee-for-service only, are now receiving additional per member per month payments (PMPM). Others are receiving payment incentives tied to performance metrics that measure quality, cost, or patient engagement. Medicare has been piloting various types of payment reform — ranging from pay-for-reporting to bundled payment — but the scale and spread of delivery models that tie payment to quality for all Medicare benefi ciaries is more recent.
As part of the Affordable Care Act, the Centers for Medicare and Medicaid Innovation (CMMI) is spearheading one of the most aggressive efforts in recent history to address delivery system reform. Recent passage of MACRA can help bring these efforts to scale across the entire Medicare program, and subsequently impact the broader commercial marketplace.
Payment Reform & PCMH: Value-based Purchasing in the Public and Private Sector
Because fee-for-service does not reimburse for key PCMH features — such as facilitating information sharing and care coordination with sub-specialists and hospitals, managing web-portals and personal health records, email communication and telephone visits, developing connections to community-based organizations, and integrating behavioral health — it often fails to compensate for the complete scope of services offered by a PCMH. Smaller practices with little reserve capacity are especially challenged in offering PCMH-level care without adequate financial support.
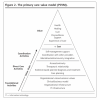
Numerous alternative payment models (APMs) are poised to support PCMH implementation and sustainability. Significant experimentation and testing of alternative payment arrangements is well underway, ranging from accountable care, to episode-based payment initiatives, to up-front payments that support primary care practice transformation, to initiatives that focus on specific populations, such as Medicaid, CHIP, or individuals dually eligible for Medicaid and Medicare.
For more information, please access our 2014-2015 PCMH evidence report.
Resources

Medicare Spending after 3 Years of the Medicare Shared Savings Program | Settembre 2018

Value-Based Care in America: State-by-State | Aprile 2019

Harvard Medical School Center for Primary Care | Luglio 2017
The model of Direct Primary Care is a subscription-based model aiming to circumvent the barriers posed by coding and payment schemes in traditional fee-for-service care. This model improves continuity as well as accessibility of care for patients. It also works to focus on the patient as a person rather than focusing on the payment scheme, making care more equitable.
American Journal of Managed Care | Agosto 2018
This resource looks at a chronic care program designed to manage patients with comorbid HIV patients enrolled in Medicaid to see how the program affected costs. The study showed that costs were reduced by over $200 per patient per month. This shows how the PCMH model can lead to higher-value, more efficient care.

Publication | Luglio 2017
- ‹ precedente
- 3 di 15
- seguente ›
News
Maggio 3, 2022 | Washington Monthly
Luglio 1, 2021 | Primary Care Collaborative
- ‹ precedente
- 3 di 68
- seguente ›
Events & Media
Luglio 10, 2019 | CMS
Giugno 27, 2019
- ‹ precedente
- 3 di 33
- seguente ›
Related Content
Pagine
Pagine
Menu secondario
Copyright © 2024 Primary Care Collaborative