Check back weekly for the latest survey results and updates.
For last week's data, see Week 8 Results.
Who replied to the survey in Week 9?
Over 2,750 primary care clinicians replied to week 9 of the survey. Internal medicine represented a much higher percentage (65%) of respondents’ specialties this week compared to previous weeks. Other specialties included family medicine (22%), pediatrics (5%), geriatrics (4%), and other (4%). Responses came in from all 50 states and Washington, D.C.; the top five reporting states were Texas (9%), California (8%), New York (7%), Oregon (5%), and Virginia (4%). Over 60% of respondents work in practices with fewer than 10 clinicians (37% with 1-3 clinicians). A large portion—27%—of responses came from clinicians working in direct primary care or a membership-based practice. Respondents were equally likely to own their practice (40%) or work for a practice owned by a hospital or health system (40%).
Responses to week 9 of the survey were collected May 8-11, 2020. Total responses: 2,774.
Results at a glance
Federal financial relief is beginning to reach primary care. A third (34%) of respondents report that they received a Paycheck Protection Program loan in the past four weeks (another third were ineligible to apply or chose not to). Fourteen percent report receiving a Small Business Administration Loan. Just over a fifth say that they received support from the federal Provider Relief Fund over the least four weeks, though the survey did not address the size of that support.
Payer support is still largely lacking. Less than a fifth of clinicians report receiving prospective payments from private insurers. More (36%) had received prospective payments from CMS, though still far from the majority. And despite encouraging steps towards telephonic payment parity, only 42% had received payment for most of their phone-based visits.
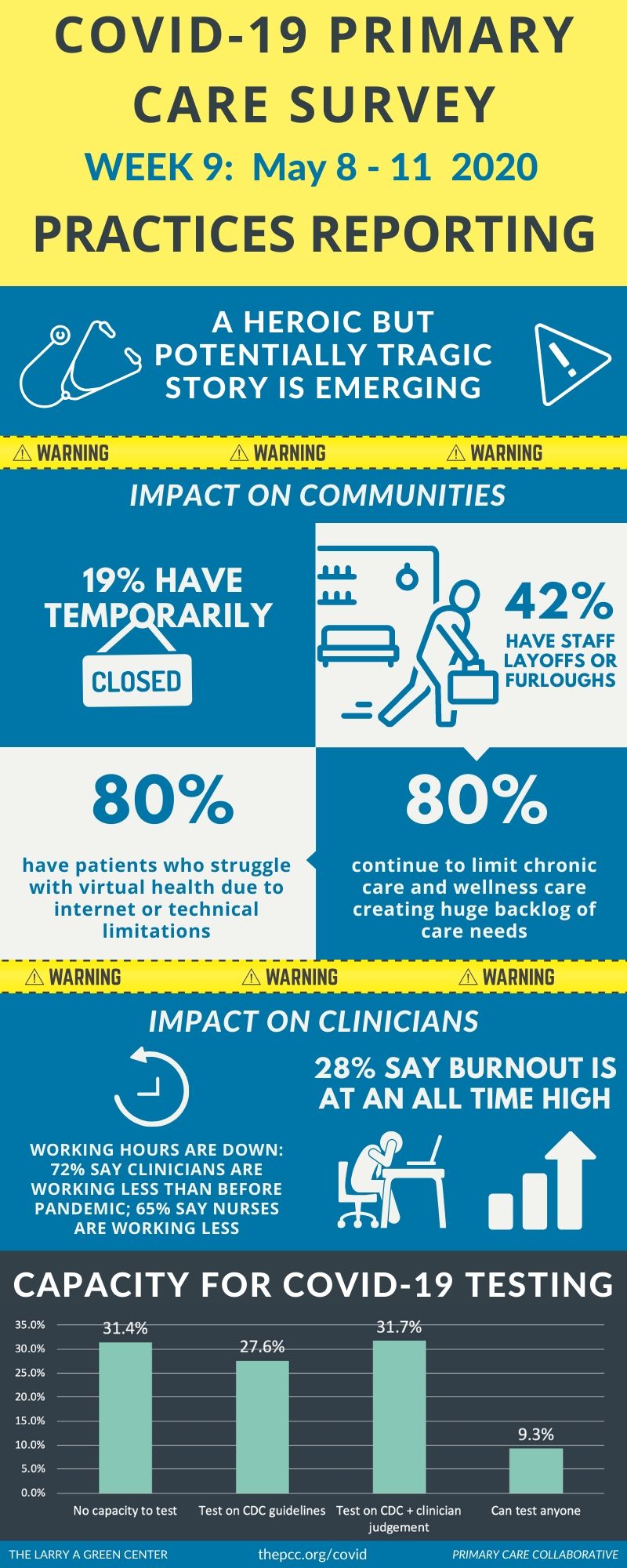
This relief is woefully insufficient, with nearly a fifth of primary care practices temporarily closed. Over 500 respondents (19%) note that their practice has temporarily closed. Another 18 (0.6%) report their practice has permanently closed. Fifty-seven percent note that payments are less than enough to cover care delivered.
The pandemic is changing the way practices function. The vast majority (79%) of clinicians reports seeing fewer patients in-person now but doing much more outreach via video and phone. Some clinicians work more on the weekends (18%) and evenings (16%) as compared to before the public health emergency; others work less (16% weekends, 26% evenings). Impact on expenses also varies: 17% say their operating expenses are less now; 39% about the same; 31% greater now.
Proactive patient care may be improving—at least for in-house care. Nearly two-thirds (61%) say they are more frequently reaching out to patients proactively as compared to before the start of the pandemic. Another 35% say they are now providing more mental health support in their practice (versus 11% who report less). By comparison, a fifth are more often referring patients to outside mental health services, while 15% are doing so less often. A third are making fewer referrals to emergency departments.
COVID-19 is impacting staffing for the worse. The majority of respondents reports that their working hours are down for all staffing types: 72% clinicians, 65% nurses, 58% administrative staff. A consistent number (42%) continue to report layoffs and furloughs of clinicians and staff. Over two-thirds say financial stress on their practice is at an all-time high, and 28% say that burnout is at an all-time high.
Learn more: Download the Green Center/Primary Care Collaborative’s Executive Summary, which includes select open-ended answers to survey questions.
Voices from the Primary Care Front Lines
Over 1,100 respondents provided open text comments in week 9.
Covid 19 is a pivotal moment for the healthcare system. My practice will be included as a casualty of coronavirus. My patients received letters this month announcing the closure of a trusted friend of 22 years. (Indiana)
Suboxone pts have de-stabilized, mental health pts have destabilized, elderly are not getting their lab work done. (Washington)
Accounts receivable almost zero; patient phone volume rising; geriatric patients cannot access technology for video visits; anxiety in the community rising; virus still rampant here. (Maryland)
The 5 owners of the practice quit taking pay for over a month. That has enabled us to keep seeing patients. We work for free basically but we are able to pay staff and their family can make it for now. (Texas)
Huge financial hardship. Every payor wants it done different, billing staff tearing their hair out. Just standardize it already! (Ohio)
Increased cost to implement regulations with decreased patient volume and reimbursement, increased use of technology burden monthly payment to use telehealth without recovering cost, monthly payment for each new technology added needs to control tech companies controlling medical practices. (North Carolina)
Devastating impact; terrified patients staying away, colleagues fighting for their professional survival, landlord demanding rent with no concessions, after being at the forefront of the AIDS epidemic with coherent leadership and brilliantly coordinated science watching the complete abdication of responsibility by the Executive/Legislative branches of gov't is an abomination. Primary care will be mortally wounded. (California)
| Attachment | Size |
|---|---|
| 152.53 KB |

Are you a physician, nurse practitioner, or PA working in primary care?
Help PCC and the Larry A. Green Center track how your practice is responding to the COVID-19 outbreak by completing the Green Center's occasional survey.
The regular surveys are no longer being conducted.
COVID-19 Updates
May 9, 2022 | Primary Care Collaborative
April 19, 2022 | Primary Care Collaborative
April 19, 2022 | Primary Care Collaborative
March 7, 2022 | STAT
February 27, 2022
- 1 of 39
- next ›

Recent News
March 19, 2024
February 28, 2024
February 22, 2024 | Conversations on Health Care
May webinar highlights: “The Commercial Market: Alternative Payment Models for Primary Care” Nate Murray explains w… https://t.co/KX9Wi2w6oY —
10 months 1 week ago
@CMSinnovates’ primary care strategy is rooted in a 2021 @theNASEM’s report which called #primarycare “foundational… https://t.co/glbPxvCysg —
10 months 1 week ago
@CMSinnovates has a new #primarycare strategy, envisioning “ACO-based primary care model tests that may focus on pr… https://t.co/aJGF1z411l —
10 months 1 week ago
- Page 1
- ››
Secondary menu
Copyright © 2024 Primary Care Collaborative