Check back weekly for the latest survey results and updates.
For last week's data, see Week 6 Results.
Who replied to the survey in Week 7?
The number of survey responses tripled this week compared to last week. Over 3,100 primary care clinicians submitted the survey in week 7. This includes approximately 1,500 nurse practitioners and 1,500 physicians, in addition to a limited number of PAs and other clinician types working in primary care. Respondents’ specialty type spanned family medicine (65%), pediatrics (12%), internal medicine (11%), geriatrics (6%), and other (7%). All 50 states and Washington, D.C., are represented in the data, with the highest number of responses coming from Texas (12% of the national sample), Oregon (6%), Virginia (6%), California (5%), and Washington state (5%). Other states with more than 100 responses include: Pennsylvania, Florida, New York, Wisconsin, and Indiana. Practices vary in terms of setting characteristics (26% rural, 16% community health center, 14% convenience-care setting, 22% direct primary care or membership) and ownership (24% self-owned, 28% independent or part of a larger group, 39% owned by hospital/health system, 7% government-owned).
Responses to week 7 of the survey were collected April 24-27, 2020. Total responses: 3,131.
Results at a glance
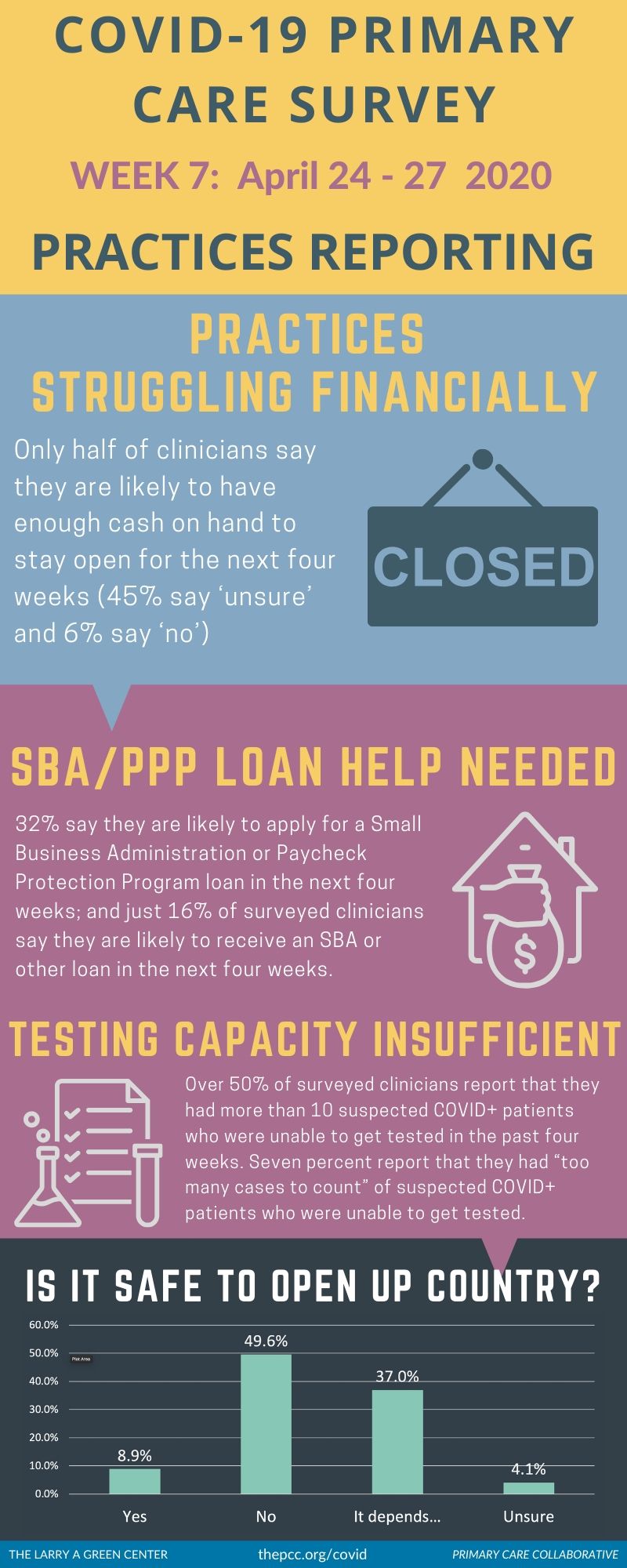
Half of surveyed primary care clinicians believe that it’s unsafe to open up the country right now, with another 37% responding that “it depends” based on testing, PPE, geographic specific conditions, etc. Only 9% responded “yes.” Eighty percent continue to limit well and chronic care visits for COVID-19-related reasons, suggesting pent-up demand for such services and population health challenges.
Primary care is playing a key role in triaging, referring, and monitoring patients. Over a fifth of respondents report that they have triaged and referred “a lot” of COVID-19-positive patients for testing over the last four weeks (14% say they’ve triaged and referred 40-99 patients; 7% say they’ve done so for 100 or more patients). Nearly a quarter (23%) report that they are monitoring many (≥40) patients at home. Yet only 52% have regular contact with their public health department, which is important for contact tracing and opening up the country.
Still, testing capacity remains insufficient in primary care practices. Over 50% of surveyed clinicians report that they had more than 10 suspected COVID-19-positive patients who were unable to get tested in the past four weeks. Seven percent report that they had “too many cases to count” of suspected COVID-19-positive patients who were unable to get tested. 32% of respondents report that their practice still has NO capacity to test for COVID-19. And just under a third believe that primary care practices should be the preferred site for testing.
Practices are struggling financially, and relief seems slow to come. Only half of clinicians say they are likely to have enough cash on hand to stay open for the next four weeks (45% say "unsure" and 6% say "no"), and only 55% say they are likely to have enough patients to stay open. Yet financial relief seems distant: 32% say they are likely to apply for a Small Business Administration or Paycheck Protection Program loan in the next four weeks; and just 16% of surveyed clinicians say they are likely to receive an SBA or other loan in the next four weeks.
Learn more: Download the Green Center/Primary Care Collaborative’s Executive Summary, which includes select open-ended answers to survey questions.
Voices from the Primary Care Front Lines
Patients’ financial and social needs are worsening, and primary care is struggling to support them
My primary focus has been on the people I care for - and the impact of this crisis on their lives has been sobering. I am dealing with medical and social needs I cannot assist with as resources are not available. The safety nets are largely broken. And yet, we are now hearing that the long-term and follow-up care for seriously ill COVID patients - after the inpatient stay - will be the responsibility of primary care practices. Where will those resources - and that training - come from when health systems are furloughing staff and cutting expenses? (Michigan)
[Many patients] live in small apartments with large families and everyone is getting sick. Even though I recommend they stay home, they go out once they feel better as they need to work. (Washington, D.C.)
Small and rural practices are not receiving the same safety, testing, and financial resources as others
We remain isolated from the rest of the state, in the northern part of New Hampshire. We are not part of the state that the officials consider when planning or a surge or included in distribution of resources such as PPE, field hospitals, personnel, or testing supplies. We feel alone. (New Hampshire)
State resources have gone to the larger entities. Small practices are left on our own to find PPE and develop policies. (Alaska)
PEDIATRICIANS have been SHAFTED. We did not get any Medicare /HHS grants ...most of us have still not got PPP/EIDL and I have to figure out how to pay for my vaccine costs ..I have high Medicaid and am rural. (Michigan)
Who else but rural care is caring for our farmers and farm communities who rely on us? We are 50 miles from any large hospital system. We have COVID 19 cases in our county an all surrounding counties and people are scared. I suspect my clinic and many others like it will have to close after this crisis is past and then what will happen to rural America? (Illinois)
Growing financial burdens for primary care practices highlight ill-fitting payment models
Telemedicine reimbursement MUST have parity with office reimbursement. I don’t want schmaltzy commercials thanking me for being a frontline hero. I want the tools to do my job- PPE, testing, tracing AND compensation. (California)
Primary care is still charged with taking care of its patients, even without office visits - and yet since we're paid based on office visits, revenue decreases while still taking care of patients over MyChart and telephone. We need more of a capitated payment plan to account for the work that PCP's do that is not face-to-face, and robust reimbursement for this work. (Wisconsin)
The pandemic continues to take an emotional and mental toll on patients and clinicians
Access to affordable mental health care is more important now than ever. Something must be done to fund professional counseling services for people who have no financial resources to pay for it. (Texas)
I am seeing significant impact on mental and emotional health. For example, people dying in a nursing home alone without their family there. The same with births. Humans are social and need to be together during life transitions. These moments are causing anxiety, immense regret, and depression. We are seeing an increase in request for medications because of this. (Arizona)We are not talking enough about the mental and emotional impact of this pandemic. (Oregon)
| Attachment | Size |
|---|---|
| 135.97 KB | |
| 376.32 KB |

Are you a physician, nurse practitioner, or PA working in primary care?
Help PCC and the Larry A. Green Center track how your practice is responding to the COVID-19 outbreak by completing the Green Center's occasional survey.
The regular surveys are no longer being conducted.
COVID-19 Updates
May 9, 2022 | Primary Care Collaborative
April 19, 2022 | Primary Care Collaborative
April 19, 2022 | Primary Care Collaborative
March 7, 2022 | STAT
February 27, 2022
- 1 of 39
- next ›

Recent News
March 19, 2024
February 28, 2024
February 22, 2024 | Conversations on Health Care
May webinar highlights: “The Commercial Market: Alternative Payment Models for Primary Care” Nate Murray explains w… https://t.co/KX9Wi2w6oY —
10 months 1 week ago
@CMSinnovates’ primary care strategy is rooted in a 2021 @theNASEM’s report which called #primarycare “foundational… https://t.co/glbPxvCysg —
10 months 1 week ago
@CMSinnovates has a new #primarycare strategy, envisioning “ACO-based primary care model tests that may focus on pr… https://t.co/aJGF1z411l —
10 months 1 week ago
- Page 1
- ››
Secondary menu
Copyright © 2024 Primary Care Collaborative