Check back weekly for the latest survey results and updates.
For last week's data, see Week 5 Results.
Who replied to the survey in Week 6?
The Week 6 survey received over 1,000 responses from 48 states and Washington, D.C. The highest number of responses came from Texas (24%), Vermont (17%), Colorado (11%), and Washington state (10%). The clinical specialty breakdown resembled past weeks, though with somewhat higher representation of pediatric clinicians: family medicine (69%), pediatrics (14%), internal medicine (12%), geriatrics (4%), and other (3%). Practice settings varied, with about a third of practices owned by the respondent; just over a quarter “independent or part of a larger group”; and 42% owned by a hospital or health system. Ten percent of clinicians work in a convenience care setting described as retail, urgent, or walk-in. A fifth of respondents work in a rural setting.
Responses to week 6 of the survey were collected April 17-20, 2020. Total responses: 1,047.
Results at a glance
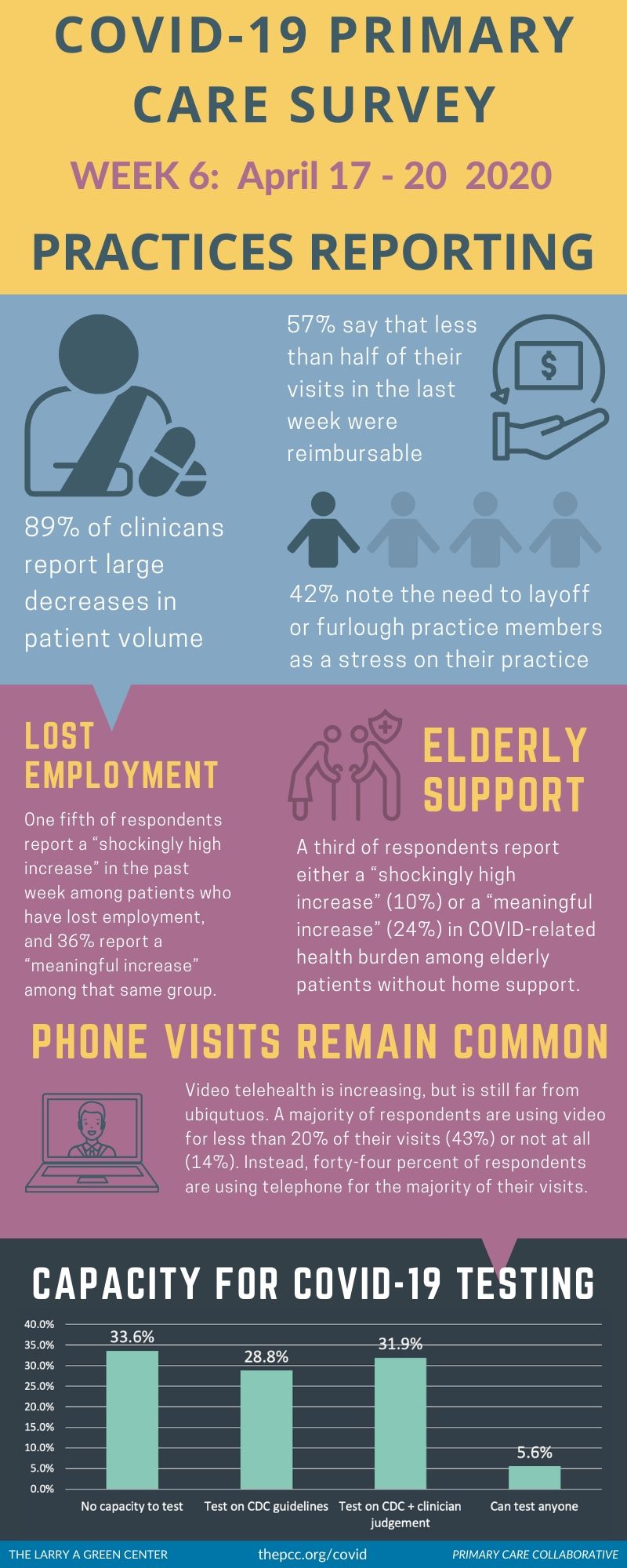
The primary care picture remains grim: Low patient volume and inconsistent reimbursement are hampering cash flow, resulting in furloughs and layoffs; PPE remains depleted; and practices are serving patients with increasing COVID-19-related health burdens—particularly among those who have lost employment or have pre-existing mental health concerns.
Vulnerable populations are observed as experiencing a noticeably larger COVID-19-related health burden.
-
Lost employment—One-fifth of respondents report a “shockingly high increase” in COVID-19-related health burdens in the past week among patients who have lost employment, and 36% report a “meaningful increase” among that same group.
-
Elderly without support—A third of respondents report either a “shockingly high increase” (10%) or a “meaningful increase” (24%) in COVID-19-related health burdens among elderly patients without home support.
-
Mental illness—Over half of all respondents report either a "shockingly high increase" (10%) or a "meaningful increase" (45%) in COVID-19-related health burdens among patients with pre-existing mental health conditions.
Clinicians often lack a complete picture of how the crisis may be disproportionately impacting different patient groups. Depending on the patient group being asked about, anywhere from 31% to 63% of clinician respondents report that they were unsure of, or had “no way to know”, the group’s increased COVID-related health burden.
Practices continue to falter under depressed patient volume and unreimbursable care. 89% of clinicians report large decreases in patient volume, and 57% say that less than half of their visits in the last week were reimbursable. 42% note the need to layoff or furlough practice members as a stress on their practice.
Other continuing strains on practices include personal protective equipment and clinician/staff absences. Over half of respondents (54%) report the use of “used and homemade PPE” and 41% report stress on their practice due to clinicians (e.g., MDs, DOs, NPs, PAs) and nursing staff (e.g., RNs, LVNs, Mas) being out due to illness or self-quarantine.
Video telehealth is increasing, but is still far from ubiquitous. A majority of respondents are using video for less than 20% of their visits (43%) or not at all (14%). Instead, 44% of respondents are using the telephone for the majority of their visits.
Learn more: Download the Green Center’s Executive Summary, which includes select open-ended answers to survey questions.
Voices from the Primary Care Front Lines
The pandemic’s financial strain on practices is continuing, and current stopgaps are not enough
Only a small amount utilizing telehealth. Office could potentially close. We have not been able to sign up for Cares due to bank site crashing. (Pennsylvania)
After working 14 years, I am furloughed. 15 NP/PAs and 46 employees furloughed in a rural setting; one clinic closed. (Michigan)
Providers caring for children are the ONLY group that received absolutely no Federal support. (Rhode Island)
Large furloughs for front desk staff, all employees have lost their employer paying into retirement accounts, no clear path to reopening clinic for more in-patient visits (we are encouraging most patients to schedule by telehealth). (Colorado)
Payers are slowly or inadequately reimbursing for telehealth
Random insurance guidelines are impossible to navigate re telehealth. We are doing and hoping for payment. (Colorado)
…I have possibly a month left of funds. I have decreased office hours, furloughed my employee. Insurers are delaying payments that I need to keep my office open. (Texas)
Reimbursement rates for telehealth do not equal an in person visit and should. (Pennsylvania)
Older patients have no or limited access to internet and devices. Reimbursement for visits low or non-existent to date. (Arkansas)
Concerns are heightening over deferred patient care
I worry about chronic illness unattended as a result of lack of access to "non-essential" care. I am imagining that next year we will be seeing increasing morbidity and mortality from cancers undetected, blood pressures out of control, etc. (California)
One type of patient care that increased was people with dental issues who can't reach their dentist. (Ohio)
Lack of ability for specialist to see patients per my referral. Patient in atrial fib can’t see cardiologist; patient with an abscess can’t see a surgeon. Offices closing and sending patients to the ER – that is not appropriate to ER. (Maryland)
| Attachment | Size |
|---|---|
| 134.56 KB | |
| 201.75 KB |

Are you a physician, nurse practitioner, or PA working in primary care?
Help PCC and the Larry A. Green Center track how your practice is responding to the COVID-19 outbreak by completing the Green Center's occasional survey.
The regular surveys are no longer being conducted.
COVID-19 Updates
May 9, 2022 | Primary Care Collaborative
April 19, 2022 | Primary Care Collaborative
April 19, 2022 | Primary Care Collaborative
March 7, 2022 | STAT
February 27, 2022
- 1 of 39
- next ›

Recent News
March 19, 2024
February 28, 2024
February 22, 2024 | Conversations on Health Care
May webinar highlights: “The Commercial Market: Alternative Payment Models for Primary Care” Nate Murray explains w… https://t.co/KX9Wi2w6oY —
10 months 1 week ago
@CMSinnovates’ primary care strategy is rooted in a 2021 @theNASEM’s report which called #primarycare “foundational… https://t.co/glbPxvCysg —
10 months 1 week ago
@CMSinnovates has a new #primarycare strategy, envisioning “ACO-based primary care model tests that may focus on pr… https://t.co/aJGF1z411l —
10 months 1 week ago
- Page 1
- ››
Secondary menu
Copyright © 2024 Primary Care Collaborative