Check back weekly for the latest survey results and updates.
For last week's data, see Week 3 Results.
Who replied to the survey in Week 4?
Over 1,000 primary care clinicians responded to the survey in week 4. Responses spanned 49 states, Washington, D.C., and Puerto Rico, with the largest percentage by far coming from Washington state (27.6% of total responses). Other states with 40 or more responses included California (8.7%), Texas (4.2%), and Pennsylvania (3.9%). Family medicine continued to be the dominant specialty among respondents (71%), followed by pediatrics (11%), internal medicine (8%), geriatrics (6%), and primary care pharmacy (1%). A third of responding clinicians work in practices where half or more of the patient population is covered by Medicaid, and about a fifth (22%) work in rural practices. Payment types varied: a third reported that the majority of their practices’ office visits last week were fee for service; 12% reported that the majority were capitated (excludes those that marked “unsure”).
Responses to week 4 of the survey were collected April 3-6, 2020.
Results at a glance
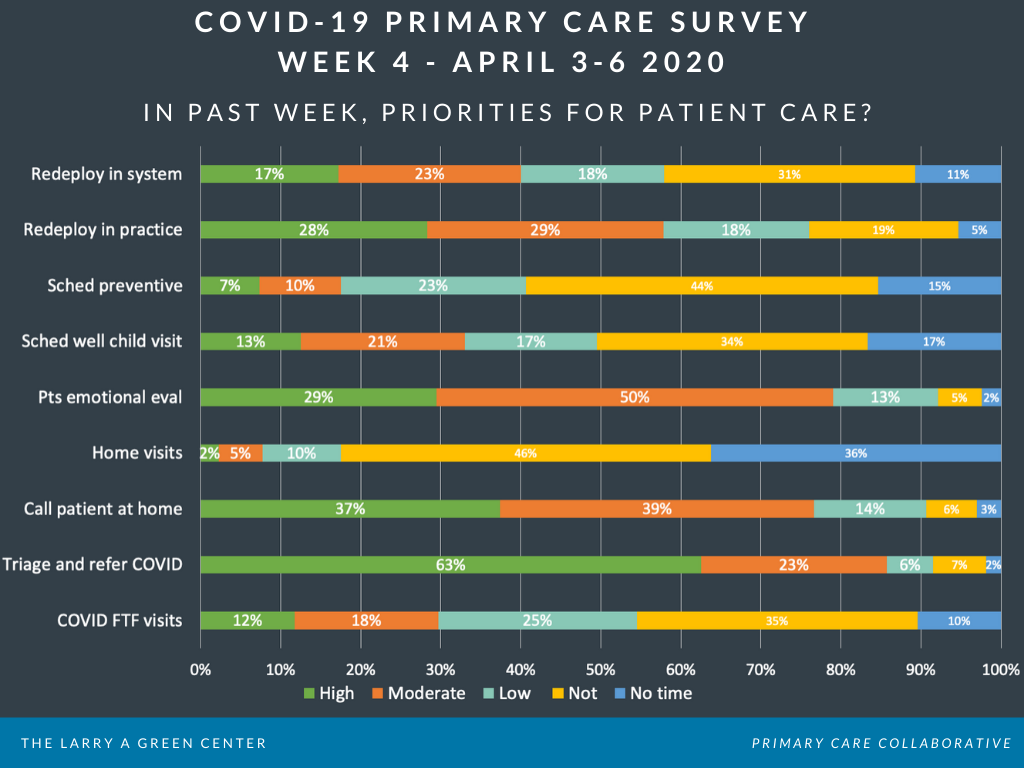
The latest round of results newly highlight key areas of focus: as telehealth becomes the new norm, many patients are unable to access virtual platforms; patients’ mental health needs are an increasing priority for care; and the primary care workforce is being redeployed to new roles, both inside practices and within the larger health system.
Nearly three-quarters of respondents report patients’ inability to use telehealth as a stress on their practice. 72% of surveyed clinicians say that they have patients who are unable to access telehealth due to no computer/internet.
Patient mental health is being recognized as a critical need. 54% report that COVID-19 has led to increased numbers of patients with mental or emotional health needs. The vast majority of surveyed clinicians report that evaluating patients’ psychological/emotional concerns as either a high (30%) or moderate (50%) priority for patient care.
The primary care workforce is being redeployed to new roles. Over half of respondents report that redeploying clinicians or staff to new roles within the practice as a high (28%) or moderate (30%) priority for patient care. Redeploying them to other parts of the health system was also a priority, but to a lesser extent: 17% high priority; 23% moderate.
After a month of urgent COVID response, a new, stressful normal may be taking hold: primary care practices continue to face an inability to test for the virus; clinicians and staff lack PPE; preventive and chronic disease visits are significantly hampered; and billing challenges pose ongoing financial strain.
Over a quarter (29%) of clinicians work at practices with NO capacity to test for COVID-19. Another 39% can test for the virus only according to CDC guidelines/restrictions. Only 3% can test for any reason.
Despite increasing billing flexibilities, primary care is facing payment challenges. Only 54% of respondents say that the majority (>50%) of their office contacts last week were reimbursable (excludes those that marked “unsure”).
COVID screening and care continues to hamper other primary care services. 90% of those surveyed report limited well and chronic visits as a stress on their practice; 58% report that they have too few sick visits available for patients. Only 7% report “scheduling preventive visits” as a high priority in the past week.
Adequate personal protective equipment remains a critical obstacle for primary care staff. 58% report the use of used and homemade PPE at their practice.
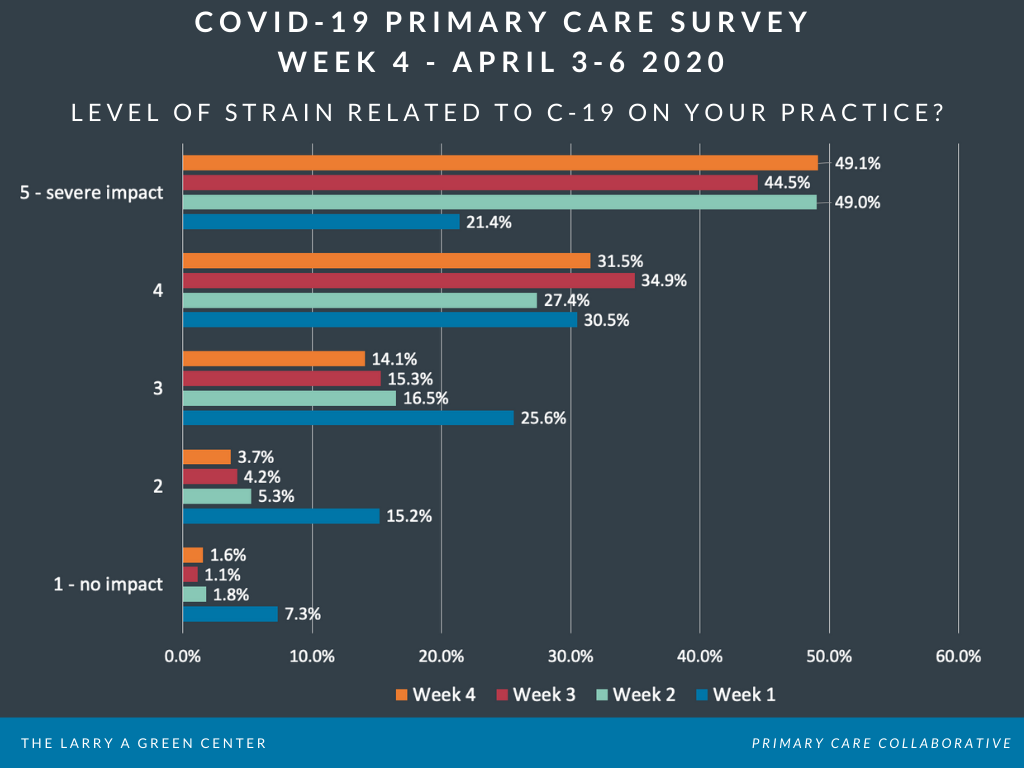
The pandemic continues to place high levels of strain on primary care practices. Just under half (49%) of respondents report that the current status of COVID-19 is having a “severe” impact (level 5 on a 5-point scale) on their practice. This is up from 44% the week before.
Voices from the Primary Care Front Lines
419 respondents included open text comments. Among these:
43% revealed tremendous financial strains threatening practice closures
"We’re holding out for a stimulus loan to stay open. If we don’t get it we’ll likely close our practice. Every day we go into work wondering if [if we’ll have a job] the next day. The red tape to get aid may be the reason we have to shut down." (Arizona)
"Extremely difficult to balance caring for patients and not risking exposure. Severe drop in all visits has become a financial disaster and may put a 25-year practice of 22 physicians and 100 staff out of business." (Florida)
"My revenue is down by 80% because my health system is not allowing us to bring in any non-urgent visits such as wellnesses, well child checks, or physicals. My health system is ALSO not allowing us to bring in ANY patients with any respiratory symptoms whatsoever. It is a very depressing time for me right now because I continue to have lots of administrative, unpaid work." (Indiana)
"We are considering closing. It’s not financially viable; we’re afraid of getting infected or [infecting] family members." (New York)
56% share high levels of stress related to difficulty with virtual health, ill-fitting policies and lack of PPE
"Despite state mandate for full coverage of telephone visits at the same rate as office visits, insurer computer systems are not equipped to pay for telephone visits; for 3 weeks 98% of our visits have been phone and we’ve not been paid." (Massachusetts)
"The crisis highlights the uselessness of the 3-day qualifying [hospital] stay; the absence of insight at CMS re older people's ability to access telehealth technology, and their ability to double the workforce by eliminating E&M coding." (Florida)
"Patients most vulnerable do not have capabilities for virtual visits. We contact them via phone - not getting reimbursed." (Iowa)
Growing concerns about unmonitored chronic conditions, reduced preventive care, and other non-treatment issues
"I work at a rural community outreach clinic. ED's are turning away pts that need to be seen for pneumonia if no underlying med conditions. They are so focused on potentially severely sick COVID-19 pts, they are forgetting to treat other conditions." (Idaho)
"Our ability to manage our complex older patients is complicated by limitations on available urgent care resources, difficulty in scheduling any needed testing, lockdowns in assisted living, and their limited ability to participate in telehealth." (Michigan)
"Babies need their immunizations but parents are afraid to come in; I am worried kids will get sick from vaccine-preventable diseases. Second concern: how will we handle the huge backlog of care needed once this crisis abates?" (North Carolina)
Learn more: Download the Green Center’s Executive Summary, which includes select open-ended answers to survey questions.
| Attachment | Size |
|---|---|
| 156.3 KB |

Are you a physician, nurse practitioner, or PA working in primary care?
Help PCC and the Larry A. Green Center track how your practice is responding to the COVID-19 outbreak by completing the Green Center's occasional survey.
The regular surveys are no longer being conducted.
COVID-19 Updates
May 9, 2022 | Primary Care Collaborative
April 19, 2022 | Primary Care Collaborative
April 19, 2022 | Primary Care Collaborative
March 7, 2022 | STAT
February 27, 2022
- 1 of 39
- next ›

Recent News
March 19, 2024
February 28, 2024
February 22, 2024 | Conversations on Health Care
May webinar highlights: “The Commercial Market: Alternative Payment Models for Primary Care” Nate Murray explains w… https://t.co/KX9Wi2w6oY —
10 months 1 week ago
@CMSinnovates’ primary care strategy is rooted in a 2021 @theNASEM’s report which called #primarycare “foundational… https://t.co/glbPxvCysg —
10 months 1 week ago
@CMSinnovates has a new #primarycare strategy, envisioning “ACO-based primary care model tests that may focus on pr… https://t.co/aJGF1z411l —
10 months 1 week ago
- Page 1
- ››
Secondary menu
Copyright © 2024 Primary Care Collaborative