- More than 200 healthcare organizations have signed on to a joint vision for primary care transformation that prioritizes coordinated, data-driven, and team-based services, says the Patient Centered Primary Care Collaborative (PCPCC).
With an emphasis on population health management, patient and provider satisfaction, community integration, and accountability, the Shared Principles of Primary Care build upon the 2007 Patient-Centered Medical Home Joint Principles to provide a guiding framework for the provider community.
“The primary care community is implementing models that deliver value – better patient outcomes, lower costs, healthier Americans, and clinicians who find joy in their work,” said PCPCC’s President and Chief Executive Officer, Ann Greiner.
Payers, providers, vendors, academic organizations, and professional societies including Aetna, the American Academy of Family Physicians, American Academy of Pediatrics, NCQA, Blue Cross Blue Shield Association, CVS Health, IBM, Merck, and Harvard Medical School Center for Primary Care have all signed the pledge to create a better primary care system.
“The Shared Principles is a powerful framework to move the United States toward a vibrant future of person-centered, team-based, community-aligned primary care, said Glen Stream, President and Board Chair of Family Medicine for America’s Health (FMAHealth), which helped to develop the framework.
“We are proud to work with PCPCC to develop these principles that can serve as a guiding light for our collective advocacy for even better primary care.”
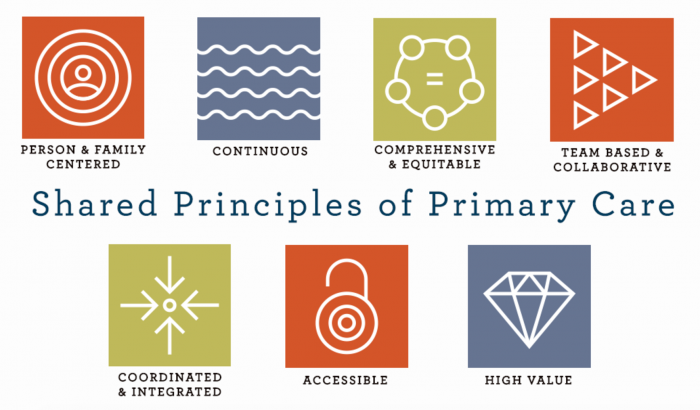
The seven founding principles of primary care transformation including creating a person and family centered ecosystem that integrates physical, mental, and behavioral healthcare with a culturally sensitive approach to holistic patient management.
“Primary care is grounded in mutually beneficial partnerships among clinicians, staff, individuals and their families, as equal members of the care team,” PCPCC says. “Care delivery is customized based on individual and family strengths, preferences, values, goals and experiences using strategies such as care planning and shared decision making.”
Other key aspects of the ideal primary care environment include reducing disparities in health equity, creating a seamless care continuum, focusing on collaboration, enhancing accessibility for all individuals, and creating a high-value experience for providers and patients.
“The Shared Principles prove there is unity and consensus on the ideal future of primary care,” said Jill Hummel, President & General Manager of Anthem Blue Cross Blue Shield of Connecticut.
“This common vision must now be supported by enablers, including alternate payments models that move away from fee-for-service, to ensure that primary care has the resources necessary to deliver on these ideals and achieve the goals of better health, better care, and lower costs.”
Recent News
March 19, 2024
February 28, 2024
February 22, 2024 | Conversations on Health Care
Missed our May webinar, “The Commercial Market: Alternative Payment Models for Primary Care,” check out this clip!… https://t.co/mDZH3IINXK —
10 months 1 week ago
Did you catch @CMSinnovates' new #primarycare strategy? Thanks to concerted efforts from @NAACOSnews and other memb… https://t.co/mDnawqw8YW —
10 months 1 week ago
Not up to date on the #Medicaid Access and #Managedcare proposed rules important for #primarycare? No worries,… https://t.co/qB6sY3XCZ1 —
10 months 1 week ago
Secondary menu
Copyright © 2024 Primary Care Collaborative



